One of the reasons that we built HealthPlanView was to redefine how account management and senior Market Access executives assess the value of the access and coverage that health plans are delivering. Most pharmaceutical manufacturers have a singular focus on Rx volume, delivered with little consideration of how that volume is derived. Rebates seldom consider the nuances of benefit designs and how patients seldom pay the copays that manufacturers contract for because of deductibles.
The first question that we redefine the answer to with HealthPlanView™ is:
What is your Access Objective?
Typically manufacturers couch this answer in the form of % of lives with Preferred Access, % of lives with Non-Preferred Access, etc. HealthPlanView™ looks at this question differently. Instead of these traditional responses, we might answer this question as follows:
|
Deductible <$2,000 |
Deductible $2,000-$3,000 | Deductible $3,000-$4,000 | Deductible >$4,000 |
Total |
|
| Preferred |
13% |
4% | 4% | 11% |
32% |
| Non Preferred |
23% |
9% | 7% | 14% |
52% |
| Specialty |
0% |
0% | 0% | 0% |
0% |
| Not Covered |
6% |
3% | 2% | 4% |
15% |
| Total |
42% |
16% | 13% | 29% |
100% |
We look at the market this way because the value of tier placement can be relatively limited when a deductible covers a significant portion of the annual cost of a drug and the value of a lower copay only applies to a small number of prescriptions during the plan year. The other side of this equation limits the application of the copay to a one or two prescriptions – which is the case with many specialty drugs that cost thousands of dollars annually. Below is another example of how deductibles can dramatically affect patient out-of-pocket costs. Here you can see two different plans within Aetna of California where Farxiga is covered at the same tier (Non Preferred), but differences in deductible and cost sharing results in more than a $5,000 difference in patient cost burden for a year of therapy ($860 vs. $6,240). 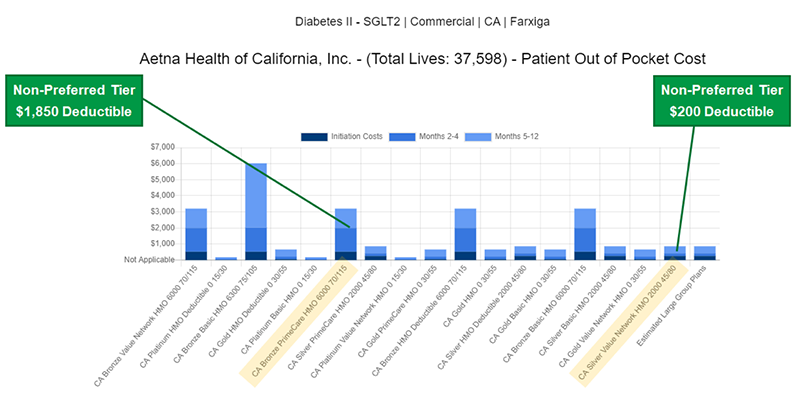 It’s become clear to us that the evolution of benefit designs argues for a new way to analyze the distribution of rebates to payers, which brings us to our second question:
It’s become clear to us that the evolution of benefit designs argues for a new way to analyze the distribution of rebates to payers, which brings us to our second question:
Which Payers are most important to us?
Traditionally, the answer to this question has been structured as a lives-based analysis juxtaposed against Rx data. Our perspective on this is a little different. We prioritize payers based on the following criteria:
- Relative ranking of payer benefit designs vs. competitors
- Relative ranking of Utilization Management criteria
- Lives-weighted average out-of-pocket cost to patient
We use these criteria and ask our clients to overlay their Rx volume data on top of these metrics because payers that rank favorably on these benefits provide greater access to patients. If Rx volume follows this access, we believe that these payers should be rewarded on a relative basis at a greater rate than other payers who measure less favorably on these metrics. We refer to this distinction as the difference between paying for access vs. paying for distribution, the latter referring to the ability of payers to provide patients the true ability to receive these treatments. Our final question addresses the disconnect between favorable access and pull-through:
Where should we be optimizing pull-through and, if we aren’t, why?
We look at these criteria to assess pull-through:
- % of preferred access in low deductible plans
- Relative ranking of Utilization Management criteria
- Insured Lives Volume
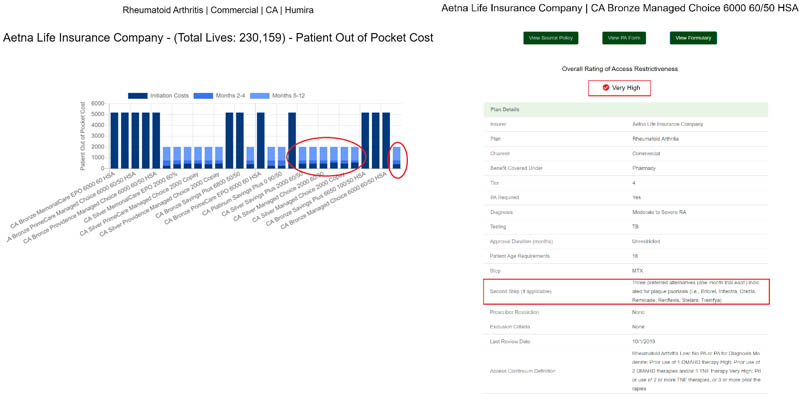 When we see a plan with High Restrictiveness and a large swath of low deductible benefit designs (circled bars on the left), we immediately assess its’ relative pull-through vs. plans with less favorable benefit designs to understand how much ‘bite’ the plan’s utilization management restrictions have. Taken together as a diagnostic tool, these criteria can be combined with prescription volume data to assess execution issues at the field and support services level.
When we see a plan with High Restrictiveness and a large swath of low deductible benefit designs (circled bars on the left), we immediately assess its’ relative pull-through vs. plans with less favorable benefit designs to understand how much ‘bite’ the plan’s utilization management restrictions have. Taken together as a diagnostic tool, these criteria can be combined with prescription volume data to assess execution issues at the field and support services level.
If you are interested to learn more about HealthPlanView, contact Nicole Espinoza, VP, Knowledge Management at Nicole.Espinoza@pharmspective.com
